Using radio-antennas for contactless monitoring of cardiac function
Radio-frequency (RF) antennas can be used as external non-contact sensors to sense physiological motion inside the human body. When an RF antenna is placed on the body and electromagnetic waves are emitted into the body, a tiny fraction of those waves is scattered back into the antenna. The amount of backscattering depends on the properties of the tissue close to the antenna. When these properties change due to physiological motion, the backscattered RF waves change 1–3 . An RF antenna can thus be used as a non-invasive motion sensor in combination with a detection device such as a network analyzer.
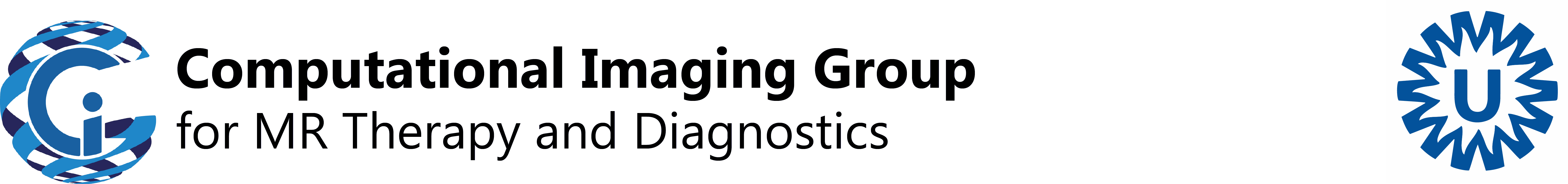
The aim of the RF Sensing (RFS) project is to measure and assess cardiac biomarkers such as ventricular volume with wearable RF antennas to detect deterioration of heart failure. By using the same type of RF antennas that are used in MRI, useful physiological information can be derived from MRI scans to improve the precision of our measurements. Figure 1 shows a prototype of the RFS with a wearable miniature network analyzer and preliminary validation data.
Figure 1: 1a. Current RFS prototype (1a and 1b) and preliminary data showing sensitivity to cardiac volume (1c).
Radio-frequency based imaging
By using an array of multiple RF antennas and acquiring data in a wide frequency band, cardiac motion can be localized to space. By using machine learning based reconstruction algorithms, 3D images of the heart can be made. Preliminary results indicate that RFS can be used to obtain images of the heart in 3D, as compared against MRI:

Figure 2: 3D visualization of the difference in dielectric properties between diastole and systole from segmented MRI (top) and from RFS (bottom).
Funding
This work was funded by an internal Circulatory Health Seeding Fund, NWO Open Mind grant 18802, NWO Take off grant 19609, an Utrecht Holdings Innovation Voucher, a DCVA Valorization Voucher, the Dutch heart Foundation Dekker Postdoc grant 03-006-2022-0024 and a HealthHolland TKI grant 2311.
Relevant publications
- A. Andreychenko, B. Denis de Senneville, R. J. M. Navest, R. H. N. Tijssen, J. J. W. Lagendijk, and C. A. T. van den Berg, “Respiratory motion model based on the noise covariance matrix of a receive array” Magn Reson Med, vol. 79, no. 3, pp. 1730-1735, Mar 2018, doi: 10.1002/mrm.26775.
- R. J. M. Navest, S. Mandija, A. Andreychenko, A. J. E. Raaijmakers, J. J. W. Lagendijk, and C. A. T. van den Berg, “Understanding the physical relations governing the noise navigator” Magn Reson Med, vol. 82, no. 6, pp. 2236-2247, Dec 2019, doi: 10.1002/mrm.27906.
- B. R. Steensma, C. A. Louka, A. J. E. Raaijmakers, and C. A. T. van den Berg, “Measuring stroke volume with wearable RF antennas: a validation study with EM simulations and MRI” in Conference of the International Society of Magnetic Resonance in Medicine, London, 2022, 31 ed., p. 3952.
- E. F. M. Meliado, C. A. Louka, C. A. van den Berg, and B. R. Steensma, “Dynamic imaging of the heart from scattering parameters using deep learning – an MR based feasibility study” in ISMRM, Singapore, 2024, p. 8140.